Palpitations are one of the most common reasons that I see patients in the inpatient and outpatient setting. Palpitations are abnormal the sensation of your heart beating. I explain them briefly in this TikTok video:
Depending on the underlying diagnosis they can be completely benign or potentially life-threatening. I go into much greater detail in a much longer separate YouTube video here:
To understand the common tools we use to diagnose and treat palpitations you have to find out how frequently they occur. So let’s review the most common tools cardiologists use to evaluate palpitations.
If they’re happening right now- get an ECG! Sometimes an Apple Watch can even diagnose some abnormal heart rhythms like atrial fibrillation. But if palpitations are not happening when you get the ECG then you will not catch the rhythm. In the inpatient setting we often also use telemetry. This also underpins the importance of talking to patients to evaluate how frequent palpitations occur as different tools can be used for different durations of time. Sometimes even when we diagnose certain abnormal heart rhythms we use the next few tools to quantify the ectopic burden (how many extra beats are there) as this may influence treatment.
Holter Monitor: 24 – 48 hours
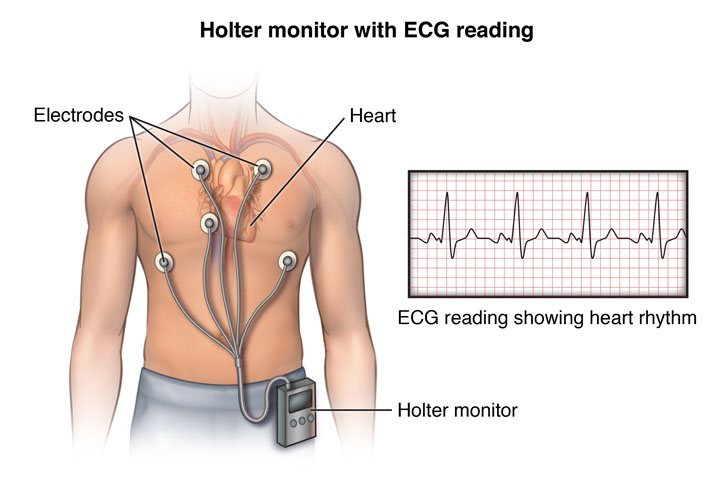
Holter monitors are 24-48 hour mini ECG’s, as depicted above. Patients wear them and document when they feel symptoms and we correlate the information we collect from the monitor. This can also help quantify how frequently someone is having a known abnormal heart rhythm to help guide other treatment choices.
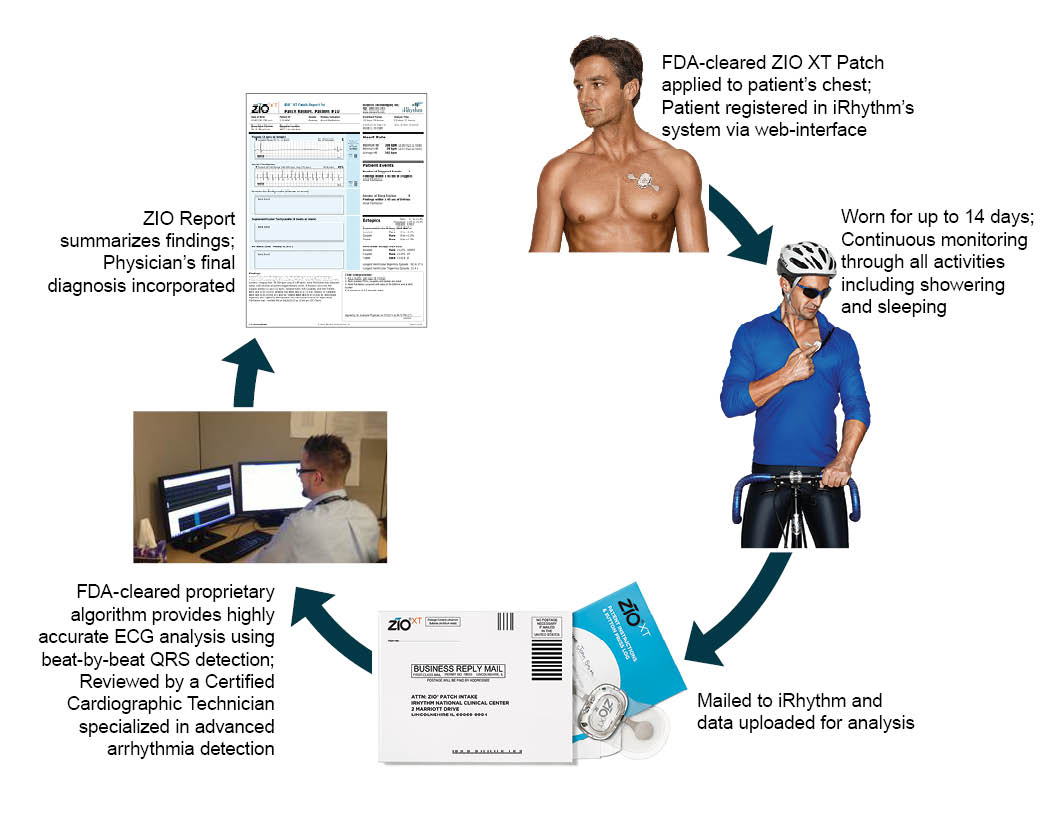
ZioPatch Event monitor: 1 – 2 weeks

Event monitors are the next step up in duration. They can be worn for extended period of time, typically for 1-2 weeks. My favorite is the ZioPatch, shown above. It can be worn for weeks at a time (again, typically 1-2) and is small, goes on the chest, and records everything while being worn, and patients can even shower with this device. They click a button on the device to note when symptoms occur and then we go back to see what rhythm was happening at that time when we receive the report. It does not get transmitted in real time. Instead, as shown below, patients actually take it off at home and send it back to the company in the mail who then forward a report to the ordering physician.
Implantable Loop Recorder: up to 3 years

Lastly are implantable loop recorders (ILR). ILRs are less than 2 inches long and quite thin, as depicted below.ILRs are the only monitoring device that is actually implanted under the skin on the chest. They record everything and have up to a 3 year battery life! The ILR automatically records certain fast and slow rhythms but patients can also use an activator to save rhythms if they’re having symptoms. We often use these when the palpitations are infrequent or if we have a high suspicion of an underlying arrhythmia without a documented diagnosis that might change management. For example, I frequently use these in tandem with neurologists in stroke patients in whom we suspect but have not diagnosed atrial fibrillation (AF). If we see AF on an ILR then we would start a blood thinner but sometimes don’t want to treat empirically. The location these are placed is shown below and often can be safely removed.
Just like any test these tools aren’t perfect. First, patients can have palpitations a few days a week but for whatever reason don’t have any symptoms when wearing the monitor. Depending on the clinical scenario sometimes we will redo the test. Second, these monitors should not be ordered unless clearly indicated. If you were to place Holter monitors on 100 random individuals you are certain to find some abnormal heart rhythms that are completely benign. Thus ordering unnecessary cardiac monitoring for patients can lead to unnecessary follow up procedures, testing, and possible harm.
If you found this helpful:

